Explainer
Blog – What’s the tea with HPV?
There’s no shame in having HPV (Human Papillomavirus).
There are over 100 types of HPV (with 40 of these affecting the genitals) and it is more than likely you know someone who has it. Almost everyone (around 90% of people) will have at least 1 form of genital HPV in their lifetime, and most won’t have any symptoms (known as being “asymptomatic”).
Here are some important facts about HPV:
- Infections usually clear in 1-2 years, but in some cases, can stay dormant in the body with symptoms reappearing in the future.
- Even if you don’t have any symptoms, you can still pass it on to sexual partners.
- Everyone who is sexually active is susceptible to HPV, regardless of the individuals or sex acts involved.
Some communities are at higher risk than others: people who are immunocompromised (including people living with HIV), and groups who experience barriers to accessing safe and affirming healthcare, such as Aboriginal and Torres Strait Islander people, people of colour (especially those from migrant or refugee backgrounds), LGBTQ+ people and people who live rurally and remotely.
The basics
HPV can affect the genitals, genital surroundings, anus, mouth and throat.
It is passed on from intimate skin-to-skin contact, meaning if you have sexual contact with someone, with or without penetration, it’s possible to pass on the infection.
If you have HPV, there’s a chance you could pass it on during sex even when you don’t have visible symptoms, although it’s less likely. You can also get HPV more than once. Remember, there are over 100 types out there!
Symptoms
Most people who get HPV won’t have any symptoms. But for those who do, symptoms are either classified as ‘low-risk’ or ‘high-risk’. Low-risk symptoms are more visible and noticeable, and cannot lead to cancer. High-risk symptoms are harder to detect, and are pre-cancerous (can turn into cancer).
Low-risk symptoms
The most well-known symptoms of HPV are genital and anal warts, diagnosed via visual examination by a healthcare provider.
Other symptoms of low-risk HPV can include:
- Painful, abnormal bleeding from genitals or anus
- Unusual pain, itching, skin changes or lumps around the genital or anal region
Warts can go away on their own, but if they don’t, there are a few treatments available to remove them. This treatment is purely cosmetic: HPV will remain in the body after the warts are removed (and can even reappear), so taking precautions during sex is still very important.
The only way to completely avoid the spread of HPV with genital warts is to not have sex when they’re visible. If you do have warts and want to have sex, practicing safer sex (that is, using condoms, barriers and lube) can help reduce the risk of transmission.
High-risk symptoms
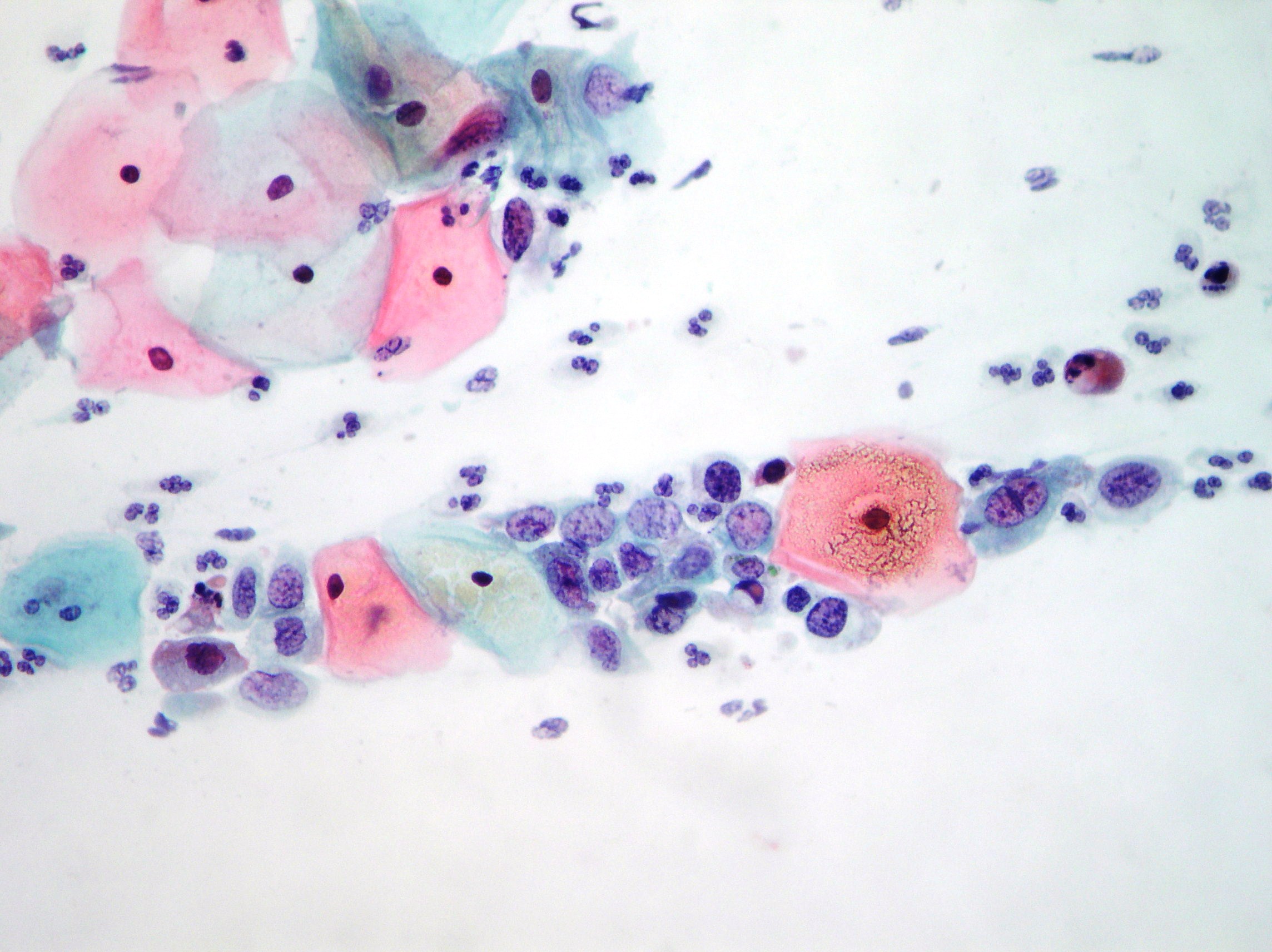
Most cervical cancers are caused by what are known as HPV types 16 and 18. They cause changes you can’t see or feel, and aren’t easily detected in a standard STI test.
These changes include the presence of abnormal, cancer-causing cells in the cervix. If HPV types 16 and 18 are caught early, they are more easily treatable. Cervical screening is available to catch these changes early.
Cervical screening
Over 70% of cervical cancers happen in people who haven’t been screened, or have missed their regular screening.
Mandatory vaccinations in schools have made the likelihood of developing cervical cancer a lot lower than it used to be. However, the best way to protect from cervical cancer is by keeping up to date with regular cervical screenings.
You are also in control of how you get screened!
Thankfully, these days cervical screening is quick and easier than ever, and you can even do the swab yourself. If results come back normal, another test isn’t required for several years. It’s important to note that self-collection tests will still be just as accurate as a screening done by a nurse or doctor.
Testing is recommended every 5 years for anyone who:
- has ever had sex (even if it didn’t involve a penis and a vagina)
- has a cervix or a neo-vagina
- is between the ages of 25-74
- is pregnant
- has been vaccinated for HPV.
Testing is recommended every 3 years for anyone who:
- is living with HIV
- is immunocompromised
- is receiving any immunosuppressive treatment.
Screening is free for most people with a cervix. For those without a Medicare card, and those not born with a cervix, there may be additional costs.
Check out CanWe for more tips on getting ready for a screening, or healthdirects service finder to see locations for getting screened.
In summary
Detecting cancer-causing HPV early means it’s more easily treatable. Detecting low-risk types can help reduce the spread to future sexual partners.
Letting partners know if you have HPV, taking precautions and getting screened are ways to take care of yourself, your lovers, and your community!
If you, a friend or a partner is overdue for a cervical screen, remember: the best way to treat cancerous strains of HPV is through early detection. So, if you want to stay cancer-free, check your vaccination records and make sure you’re up to date with screening – and that’s the tea!
Or explore more on

We’ve got you covered
Your free Play Pack includes everything for safer sex, delivered discreetly because you deserve to focus on the fun stuff.